Beginner’s Guide To Mental Health Billing for Therapists
Our Beginner’s Guide to Mental Health Billing is for the brand new and having-no-clue outpatient therapist looking to learn how to bill insurance companies. You will learn what client information you need, how to verify mental health benefits, create and submit claims, and account for EOBs.
Every mental health insurance claim will require a large amount of information, but that information needn’t be overly complicated.
Our guide to mental health billing will first discuss your client information, then the most frequently used mental health CPT codes, how to verify eligibility and benefits for behavioral health services, and finally how to submit claims.

If you know you want to work with our team of billing experts to get your problems sorted right now, simply drop us a line.
Beginners Guide Outline:
- Beginners Guide to Mental Health Billing Video
- Collect Client Demographic and Insurance Information
- Verify Mental Health Eligibility and Benefits
- Verify Claims Submission Requirements
- Create and File Claims Coded with the correct Mental Health CPT Codes
- Follow Up With Your Pending Claims
- Account For Your Payments via EOB Reconciliation
- Handle Rejections, Denials, Appeals & Submit Corrected Claims
Each of those steps aren’t exactly one step but with this comprehensive structure of how to bill mental health insurance, let’s begin!
Beginner’s Guide to Mental Health Billing Video
Link –> https://www.youtube.com/watch?v=Chmm8MCRvx0
Minimum Required Patient Information
 Required Demographic Information:
Required Demographic Information:
- Your patient’s full legal name
- Your patient’s date of birth
- Your patient’s address
- Your patient’s gender (male or female, not the most progressive)
Not Required:
- Their Social Security Number (almost never required)
- Case Notes (keep them, however, if you need to provide evidence of medical necessity)
- Their Phone Number (good idea to collect this, though)
- Their Email Address (also a good idea to collect this)
Required Insurance Information:
- Their Subscriber ID with the Alpha Prefix (always record letters and numbers in their subscriber ID, not just numbers)
Not Required:
- Group Number
That being said, we recommend snapping a front and back photo of their insurance card for your records.
Having the customer service phone number isn’t essential for submitting claims, but is necessary to gather eligibility and benefits information and to verify claim status and payment amounts.
Time to move onto mental health CPT codes.
The Three Most Often Used Mental Health CPT Codes
They are:
- 90791 – Intake session — to be billed for your first appointment with that patient exclusively
- 90834 – 45-55 Minute Individual Therapy Session
- 90837 – 56+ Minute Individual Therapy Session

It’s as straight forward as it seems: bill the intake code for their first session, and bill either a 45 minute or 60 minute session for the rest, depending on the length of their sessions.
Dealing with family therapy, therapy with a family member with the patient not present, group therapy, or other cases? Review our definitive guide to CPT codes to get sorted!
Other Common Behavioral Health CPT Codes:
- 90846 – Family or couples psychotherapy, without patient present.
- 90847 – Family or couples psychotherapy, with patient present.
- 90853 – Group Psychotherapy (not family).
- 90839 – Psychotherapy for crisis, 60 minutes (30-74 minutes).
If you are struggling to translate specific aspects of your services to ICD10 diagnosis codes and CPT codes, we are experts at helping specifically and exclusively with our mental health billing and coding service, so consider reaching out.
Telehealth Billing: Quick Guide [2021]
 With telehealth becoming a popular if not required option for conducting therapy sessions in 2020, keep note of the following four points when billing telemedical therapy appointments:
With telehealth becoming a popular if not required option for conducting therapy sessions in 2020, keep note of the following four points when billing telemedical therapy appointments:
- Pick the most appropriate CPT code for your services. Do not pick a “telehealth” CPT code. 90791, 90834, 90837 are appropriate here.
- Call the insurance plan to verify the “Place of Service Code” used for billing with that company, most often POS Code 02, and the Telehealth modifier they are using, most often GT or 95.
- Ask about telehealth benefits, especially if you are out of network.
- Make sure to submit your claims with the place of service code and modifier required by their insurance plan.
If you are struggling to find out the place of service code or modifier to use for your insurance claims, this is something we provide as part of our billing service free of charge.
Our beginners guide to mental health billing doesn’t make eligibility and benefits verification calls for you, but we do!
Choosing a Mental Health Diagnosis
We cannot and will not advice you to use a single diagnosis code, even though it is a very common practice for therapists to use one code for all of their patients (e.g. anxiety or depression).
It is your duty, as demanded by submitting any insurance claim, to submit the most accurate diagnosis you possibly can for each session. If their diagnosis changes, you need to update it on your claims forms.
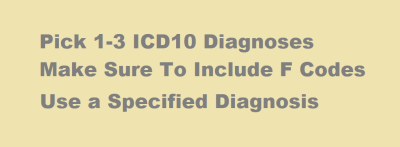
Tip: Always use a specified diagnosis. Since the ICD10 / DSM-5 change, unspecified diagnoses are being rejected by Medicare. (Source)
Otherwise, just review our ICD10 Mental Health Diagnosis Code Search Tool to pick the most accurate diagnosis.
Okay! You have all the necessary patient and session information to file claims. Now it’s time to check eligibility and benefits to ensure they have coverage that will reimburse you.
How to Check Eligibility and Benefits for Mental Health
We have a guide called “How to Check Mental Health Eligibility and Benefits” at this link which contains a script and thorough questions to ask so you gather all necessary information.
If you want the quick and dirty version, you’ll need to:
- Call the insurance card via the customer service phone number on the back of the card.
- Ask to verify mental health outpatient provider eligibility and benefits.
- Give them your NPI and Tax ID and ask if you are in-network.
- Give them the patient’s name, date of birth, and subscriber ID.
- Ask them for the patient’s deductible, copay, and coinsurance. Record them all.
- Ask for the claims addresses.
- Try not to pull out all of your hair while you do the whole thing.
- Consider reaching out if you want us to handle any or all of this for you, if the above already sounds too pain-inducing.
Okay! You now have all the necessary information to file claims, you know what to charge the patient in person, and you know where to file the claims.
Guide to Mental Health Billing: How To Submit Claims
Unfortunately, this is the extremely annoying, hard part. There is no “quick guide” way of handling this process.
The cheapest option is to learn how to use “PracticeMate” by OfficeAlly to submit claims, even though it is made for hospitals.
You can try to use a purely software solution to input the data and create the forms. You can reach out to us for help: we do every part of the billing process for you. (Not free but you may live longer without that stress).
However you end up doing them, you need to transcribe this information onto a CMS1500 form and send it electronically or physically to the insurance company.
Once you’ve done that..
Call and Verify Receipt of Claims & Payment Information
If you’ve mailed in claims, wait 4 weeks to call and verify claims are received. If they haven’t been received, verify their claims address and submit again.
 It’s critical to submit them within the 90 day timely filing window most insurance companies hold you to (not all, but most).
It’s critical to submit them within the 90 day timely filing window most insurance companies hold you to (not all, but most).
Once claims are verified as received, it’s time to hurry up and wait until payment. Often processing takes two to three weeks after receipt of the claims, plus the time to mail checks.
You will received EOBs in the mail along with a check for those dates of service.
Finish with EOB Accounting
Finally, add them to your appointment list spreadsheet or tracker, including
- check number
- patient responsibility
- amount reimbursed by insurance
- the amount you collected in session
How to Handle Mental Health Billing Denials, Rejections, and Appeals
Each denial or rejection can happen at one of two places, either at the Clearinghouse level or the insurance company level.
Use your EHR portal to determine if the claim has been denied at the clearinghouse for a missing enrollment, bad subscriber ID, or incorrectly submitted information. (We help with this).
You can ensure your claim is not denied at the clearinghouse by calling the insurance company and asking if they have the claim on file. If they do, the claim made its way through your clearinghouse. If not, you need to resolve the problem at the clearinghouse level.
If the claim is on file with insurance and is denied, you need to understand the denial reason. Is it for timely filing, terminated coverage, a coordination of benefits issue, unauthorized sessions, needing updated provider information, to just name a few denial reasons?
Go claim by claim, date of service by date of service, and refile the claims as correct with insurance.
If your claims require appeal, speak to a customer support representative about obtaining the necessary forms to file your appeal. Use your reference ID from your eligibility and benefits verification phone call to fight your case.
Fighting denials and rejections is the hardest part of billing. This is yet one more reason why mental health providers choose billing services like TheraThink to help. This is a headache you don’t deserve nor are your trained to handle. Consider outsourcing this work to experts.
Conclusion
It’s a damn shame that submitting insurance claims is such a pain.
We wish it were easier, as the whole process causes revenue loss, frustration, and inefficiency in our health care system.
That being said, if you just want to gather up your new patient’s demographic info and their subscriber ID, we can take care of the rest.
Hopefully this guide was a helpful introduction to mental health billing claims.
Please let us know in the comments how we can improve it, answer your questions, and simplify the process.


